Implementing Health and Wellbeing Conversations
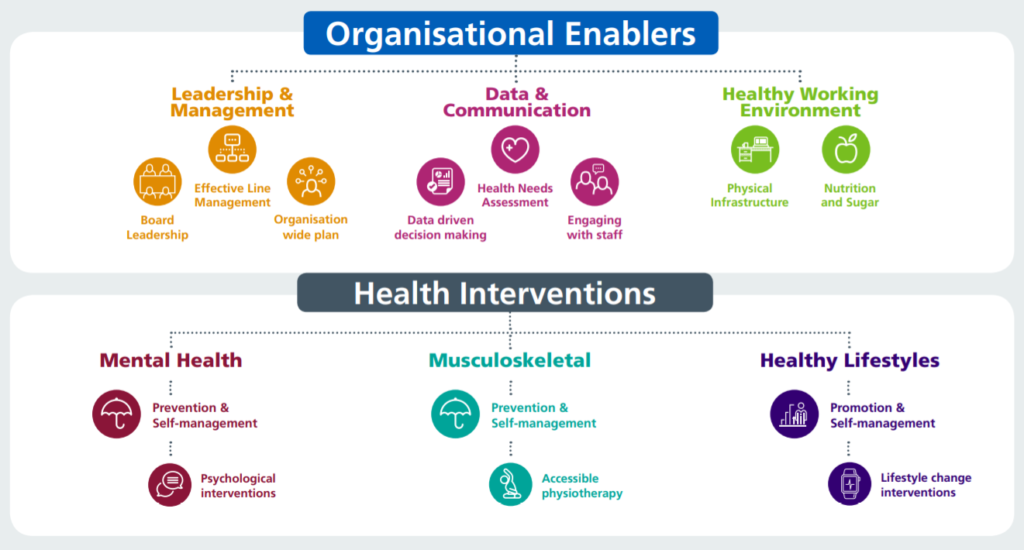
Whilst this document describes the process of implementing the Health and Wellbeing Conversations, we would also encourage organisations to consider the wider enablers that will ensure the discussions that take place have their full effect. The NHS Workforce Health and Wellbeing Framework is designed to support organisations through an improvement process to enable them to target and identify areas that need more attention to move towards a healthy workplace:
The following are critical factors that would need to be in place to have effective discussions:
Board leadership
The example needs to be set from the top. The experience of this pandemic will likely have also taken a toll on board members as well as front line staff. Board members should have their own Health and Wellbeing Conversations. All board members can also play a key role in creating psychological safety for others, promoting the message that “it is ok not to be ok” and highlighting how the experience of 2020 has affected you
Governance
Each organisation should identify:
– Responsibilities at executive and operational level for implementing the Health and Wellbeing Conversations
– Where progress on the design and roll out would be overseen in your organisation
– How your organisation will evaluate how the conversations are working, find ways to improve the process and also develop a sense of the staff wellbeing risk within the organisation
– How the board and its People sub-committee will be made aware of the level of risk emerging from the conversations.
– How safeguarding issues which may emerge from the conversations should be handled
Effective line management
Many staff may choose to have the conversation with their line manager; however, we know from the staff survey that not everyone has the kind of working relationship which would make that a comfortable conversation. The implementation plan will also need to consider a) how line managers will need to be open to and supportive if staff opt for someone other than them and b) who else might act as an alternative.We know when it comes to asking for help, the more choice people have, the better the uptake of support. Your network of trusted people will depend on who you have available to support the programme. People who might make up your Wellness Champions or Wellbeing Guardians’ groups might include:
– Local staff network leads; to help ensure the group of facilitators is diverse and inclusive, particularly for people from minority groups and those with protected characteristics
– Freedom to Speak up Guardians and champions
– Clinical supervisors
– Staff-side representatives
– Peer supporters
– Chaplaincy and other faith leaders
– Guardians of Safe Working for organisations with trainee medical staff
– Coaches or mentors
– Healthy workplace allies
Whether it is line managers or champions/guardians who facilitate the discussion, effective support for them to discharge the role key will be critical. Fundamentally, facilitators are simply asked to be supportive and compassionate; from one human to another. If people do want more training to be able to spot when someone is struggling, some options are included in the Current Resources section. It is important to consider how those facilitating Health and Wellbeing Conversations will access the right kind of support themselves. Giving others emotional time and space can be draining. Organisations will need to make sure there is clear support in place for facilitators to access help to manage this role. In your local organisation, this could include:
– Mental health professionals available to provide supervision
– Clinical or educational supervisors
– The community support available in the virtual staff common rooms, available nationally
– Internal Communities of Practise
Engagement
Each organisation will have their own view of how best to promote the offer to staff. However, the communications plan for the initiative should include:
– These are preventive conversations designed to support wellbeing and staff do not have to be physically or mentally unwell to benefit
– They are designed with everyone in mind – not just those providing direct patient care
– They are not a therapy session
– They are confidential and disclosure of information would only occur with their permission or if a safeguarding risk was identified
– Reasonable adaptations will be made for staff shielding, home working or staff with disabilities
– For those people who do not find the prospect of a conversation with their line manager comfortable, alternative facilitators will be offered
Infrastructure
Where these conversations happen is as important as when. Some things to consider, to enable all staff to participate, whether that is in person, or virtually for those shielding or working from home include:
If the conversations are held in person:
– Having neutral spaces identified may help to encourage people to engage in the offer. This includes meeting spaces that are safe, confidential and comfortable. Conversations held in managers offices might invoke feelings of anxiety, so alternatives to these will be helpful. There is some evidence to suggest green spaces support wellbeing, so also consider using green spaces in and around the working area, if these are available, appropriate and can be confidential
– How to enable appropriate and safe distancing, in line with your organisation’s protocols and advice
– How to support those that might need extra assistance or reasonable adjustments
If the conversations are held virtually:
– Enabling conversations to be held in confidence, thinking about the surroundings of those meeting in different locations
– How to support those who might need extra assistance, access to technology, reasonable adjustments etc.
– Having clear guidance that phone or video calls mustn’t be recorded
Managing referrals
Engaging your HR team and any mental health support services you have access to will help to build a strategy for managing onward referrals to further support e.g. to Occupational Health. This particularly needs to address whether or how referrals might be made by any non-line managers offering Health and Wellbeing Conversations. Where staff members need further support we know from the evidence that the more choice people have for support, the better. When it comes to onward referrals, options for facilitators of Health and Wellbeing Conversations could also include:
– Your Employee Assistance Programme (EAP)
– Local NHS and independent sector mental health providers under contract with the NHS
– Mental health charities
– People.nhs.uk national offers
– The individual’s GP and Improving Access to Psychological Therapies (IAPT) services
– Psychological support services via Occupational Health and Wellbeing Services – more information can be found at NHS Health at Work network (registration is required)
Guidance written by NHS England and NHS Improvement Mental Health will be available soon for organisations on delivering support and psychological interventions for health and care staff in response to the COVID-19 pandemic. It will provide advice on the range of services likely to be needed for staff who need treatment rather than resilience support
Managing sickness absence
Initial insights from organisations implementing The NHS Workforce Health and Wellbeing Framework show that when there is a genuine culture shift towards supporting workers to care for their health and wellbeing, there may be a small rise in sickness absence. Presenteeism declines as individuals feel more empowered to take the leave they need to get well. While an increase in sickness absence may create challenges in filling rotas or covering work, it is important to note that presenteeism has negative consequences beyond the individual staff member. Presenteeism is linked to increased risks to patient safety (Rainbow, J et. al 2019). As organisations roll out the conversations, we recommend they monitor local sickness absence rates in the areas which have gone live and consider how to mitigate staffing gaps as part of the plan part of the Plan, Do, Study, Act (PDSA) cycles